Einthoven's Triangle and the four limb leads make up the "HEXAXIAL
VIEW!" This view is a vertical/frontal-posterior - ventral/dorsal plane making
a star with 6 points intersecting through the heart in a flat frontal plane
across the patients chest.
The PRECORDIAL views are used to make up the
other six views of the heart for a total of twelve views.
So, adding this up: lead I, II and III, lead AVR, AVL, AVF, and the 6
precordial leads equals 12 leads... RIGHT?????
Correct, however, we only
need 10 electrodes placed.
( 4 on the limbs and 6 on the chest
)
The cardiac monitor uses the four Limb Leads to make up Lead I, II,
III & AVR, AVL, AVF; six views...
12 lead Quick Triage
The following situation constitutes activation of the cardiac
response team at the hospital by reporting the field diagnosis of
AMI!
- Category one: AMI that clearly meets the criteria.
- Example:
- 1 mm or more of ST elevation in the inferior leads (II, III, AVF) with
reciprocal changes in the lateral leads (I, AVL, V5, V6)
- Reciprocal changes not necessary to make the diagnosis.
- Category two: The following will result in your reporting
the specific findings of concern that may or may not result in the Cardiac
Response team.
- Example:
- 1 mm of ST elevation in the anterior leads. (V1-V4)
- Example:
- Injury/Infarct pattern in the presence of LBBB with cardiogenic clinical
presentation.
The following situation will result in the 12 Lead ECG being reported
as "normal". No subsequent activation of the cardiac response team.
- Category Three: No patterns of ischemia or infarction.
Other Signals to use as a diagnostic
tool:
- Tachycardia:
(heart rate above 100) indicates damage to the left Ventricle and an
"anterior" or "lateral" infarct. The Left Circumflex and or Left Descending
Coronary Artery is occluded.
Visable elevation in the
CHEST LEADS: V-3, 4, 5, & 6.
- Bradycardia:
(heart rate below 60) indicates damage to the Right Ventricle and an
"inferior" or "posterior" infarct. The Right Coronary Artery is
occluded.
Elevation in the LIMB LEADS: II, III,
& AFV.
Systematic Infarct Recognition
Approach
- Assure that aVR is primarily negative.
- Rule out a :eft Bundle Branch Block (LBBB) in V1 and or V2... Verify in
V6.
- Check all leads for patterns of ischemia, injury, infarction and
reciprocal changes.
AMI diagnosis criteria: 1mm. or more of ST elevation in 2
or more contiguous leads.
Anterior wall requires 2mm. or more of ST
elevation (V1-V4)
Caution: LBBB
Lead Groups
| INFARCT
LOCATION: |
ST ELEVATION FOUND
IN: |
| Anterior - Septal |
V1, V2, V3, and V4 -- 0.2mV or more in
leads |
| Posterior |
V1, and V2 -- 0.2mV or more in
leads |
| Inferior |
II, III, and aVF -- 0.1mV or more in 2
leads |
| High Lateral |
I, and aVL -- 0.1mV or more in 2
leads |
| Low Lateral |
V5, and V6 -- 0.1mV or more in 2
leads |
"ST Depression indicates Angina"
Diagrams below indicate which part the heart is being affected and
what lead would show the changes.
Reciprocal Changes
| Region of ST
Elevation |
Region of ST Depression |
| Anterior (leads V1-V4) |
Inferior (true posterior) |
| Inferior (leads II, III, aVF)
|
Anterior (leads V1-V3 or lateral lead
1. aVL) |
| Lateral ( leads I, aVF, V5,
V6) |
Inferior ( leads II, III, aVF)
|
| True Posterior |
Anterior (leads
V1-V3) |
12 lead rapid assessment
- Verify aVR is negative
- Assess rate and rhythm
- Axis determination - Leads I and aVF
- Conduction abnormalities:
- LBBB - seen in V1
Hypertrophy
Aneurysm
Pericarditis
Drugs
or
Electrolytes
Early repolarization
- Ischemia, Injury, Infarct signs:
- T-wave inversions
- ST segment elevation
- Significant Q waves
- Acute MI pattern:
- Anterior:
- ST elevation in V1, V2, V3, V4
- ST depression in II, III, aVF
Inferior: ST elevation in
II, III, aVF
- ST depression in V1, V2, V3, or I, aVL
Lateral: ST
elevation in I, aVL, V5, V6
- ST depression in II, II, aVF
Septal wall: ST elevation in
I, aVL, V1, V2
Posterior: tall and wide R waves and ST depression in
V1, V2
Right Ventricular: ST elevations in V4R, V5R, V6R
- (5 additional right chest wall electrodes placed on the chest in the
same positions as the precordial leads)
- Clinical presentation
- Treatment plan
Electrical Current:
Electricity always flows from positive to negative. The electrical
current should flow from negative to positive in the normal healthy heart. So,
if this pattern is disrupted by a "detour" or as in the heart, "an infarct" or
"injury" the ECG recording will indicate the abnormal flow of current. With an
infarcted heart, the electrical current flows opposite of where it is expected
to flow. Hence, the elevated or depressed ST segment . For instance, an inferior
infarction will show an elevation in lead II, III and aVF. The normal flow would
be "isoelectrical" and the ST segment would be equalized or level. But, since
the flow is going backwards around the damaged heart muscle, we see an elevation
on the record. It is this precise measurement that can dictate exactly where the
infarct is located. If the ST segment is elevated in V2, V3 and V4, the infarct
is anterior. These views are looking at the front or anterior area of the heart
muscle. The current is flowing toward the positive electrode on the patients
chest. When the current is disrupted, it will show as an elevation in the ST
segment versus an isoelectric reading.
Think of it like
this: An X-ray film is placed behind the heart at the area between the Ventricle
Septum. The X-Ray machine shoots the picture from the anterior heart directly
above the film. and the film captures the image. We would be looking at the area
of the heart at the Septal region which would be in ECG terminology V3.
- The infarct area will have no electrical current. The ST segment
will be depressed
-
-
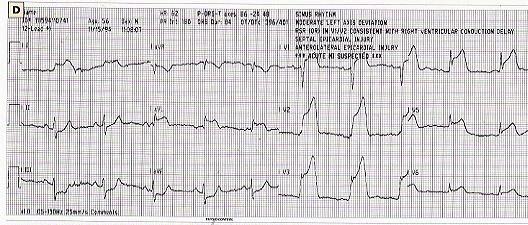
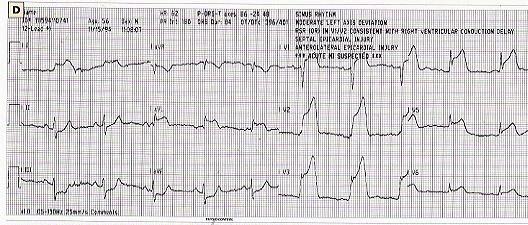
The 12 Lead Photograph
Simultaneous acquisition 2.5 seconds per view, 10 seconds for a
complete study
| I |
aVR |
V1 |
V4 |
| II |
aVL |
V2 |
V5 |
| III |
aVF |
V3 |
V6 |
12 lead ECG; a real time video recording of the hearts electrical
function.
This record indicates a "septal / anterior Infarct."
If you can comprehend which way the current is expected to flow in
The HEXAXIAL VIEW and The PRECORDIAL VIEW of the heart, then you can diagnose
which area is effected if it is an abnormal flow...
See the information
below.
12 lead rapid
interpretation
Common ECG
Formation
 |
Iscehmia=Inverted T waves
- Inverted T wave is symmetrical
- T waves are usually upright in leads I, II, and V2-V6
|
 |
Injury=Elevated ST segment
- Signifies an acute process; ST returns to baseline with time
- If ST elevation is diffuse and unassociated with Q waves or
reciprocal ST depression, consider pericarditis
- Location of injury can be determined in same manner as infarct
location
- Usually associated with reciprocal ST depression in other leads
|
 |
Infarction=Q wave
- Small Qs may be normal in V5, V6, I and aVL
- Abnormal Q must be one small square (0.04 sec) wide
- Also abnormal if Q-wave depth is greater than one-third of QRS
height in lead III
|
Making the accurate Field
Diagnosis:
- There are elevations ( 1
mm
)in two contiguous (connecting) leads:
Leads adjacent to
each other...
- There is at least one lead with reciprocal
changes..
- If the Q wave is more than 1/3 the size of the R
wave...
Table below shows what the ECG would look like in the Vector where
the heart is being affected. All other areas would look normal, without
elevation or depression. unless there is an "old MI." In that case, the prior
damage would show up as a depressed segment.
Anterior
Infarction
 |
- ST elevation without abnormal Q wave
- Usually associated with occlusion of the left anterior Descending
branch of the left coronary artery (LCA)
|
Lateral Infarction
 |
- ST elevation with/without abnormal Q wave
- May be a component of a mutiple-site infarction
- Usually associated with obstruction of the left circumflex artery
|
Inferior Infarction
 |
- ST elevation with/without abnormal Q wave
- Usally associated with right coronary artery (RCA) occlusion
|
Right Ventricular
Infarction
 |
- Usually accompanies inferior MI due to proximal occlusion of the RCA
- Best diagnosed by 1 - 2 mm ST elevation in lead V4R
- An important cause of hypotension in inferior MI recognized by
jugular venous distension with clear lung fields
- Aggressive therapy is indicated, including: reperfusion, adequate
IV fluids for right heart filling, and pacing to maintain A-V synchrony
if necessary
|
Poterior Infarction
 |
- Tall, broad (>0.04 sec) R wave and ST depression in V1 and V2
(reciprocal changes)
- Frequently associated with inferior MI
- Usually associated with obstruction of RCA and or left circumflex
coronary artery
|
Pathological Q waves:
If the Q wave ( the first downward "negative" deflected wave ) is
more than 1/3 the size of the R wave ( the first upward deflected "positive"
wave ) it is pathological and indicative of an A.M.I.
If no R wave is
recorded, then the infarct is extremely acute. There is no electrical activity
of the ventricle during polarization and contraction.
Bundle Branch
Block
In Bundle Branch Block, the firing of the Ventricles does not occur
simultaneously as it should (It occurs in series instead of parallel).
Conduction reaches a block in one of the branches (in the cardiac septum) and
refers it to the opposing branch to be conducted completely. It is then when
conduction jumps the Intra-Ventricular Septum to ultimately conduct to the
remaining blocked Bundle Branch. It is because of this that you see two
different distinctly separate QRS complexes over-lapping one another. Hence, the
"Rabbit Ear" and "RSR pattern." Remember, the QRS complex will
always be at least .12 in width and posses abnormal morphology. ALWAYS
CHECK RIGHT AND LEFT CHEST LEADS FOR BUNDLE BRANCH BLOCK (V-1, V-2,
& V-5,
V-6)
Infarction associated with a
Left Bundle Branch
Block
A LBBB may result from an acute myocardial infarction (AMI), but field
paramedics cannot diagnose AMI in the presence of LBBB. The presence of LBBB
negates meaning ful interpretation of other EKG criteria
A LBBB pattern prior to the onset of clinical findings of AMI with marked
reduction in voltage of the QRS complex may offer clues to the diagnosis of an
infarction.
LBBB obscures the pattern of AMI since the initial QRS vector is abnormally
directed in a LBBB pattern. It will obscure the infarction vector and abnormal Q
waves will not appear. The most diagnostic feature of AMI is the abnormal
direction of the initial 0.04 sec of the QRS vector (ie; the abnormal Q wave).
- LBBB is usually associated with an Inferior wall AMI when an AMI is
diagnosed.
- LBBB is usually associated with hypertensive ischemia or primary myocardial
disease.
Diagnosing the Bundle Branch Block:
Right or Left???
The last 0.04 seconds of deflection on the QRS complex is used to determine
the direction of the block.
In V1 or MCL1, if the QRS duration is greater
that 0.12 seconds (usually 0.14 - 0.20 seconds) and the last 0.04 second segment
of the complex is pointing down (negative deflection), the block is
LEFT.
If the last 0.04 seconds of the QRS complex is pointing up and is
positively deflected, the block is RIGHT.
Infarct Recognition
Some Additional Tips...
Certain easily identifiable ECG changes that are observed in the presence of
cardiogenic chest pain, reveal some strong presumptive evidence toward the
positive diagnosis of AMI. This pattern of changes is referred to as the
"evolution of Myocardial Infarction."
It is often suggested that the first observable evolutionary change is the
ischemia we associate with T-wave inversion or ST segment
depression. Then, onto what is referred as the hyperacute phase. In
the hyperacute phase of the MI, (usually the first few minutes) the T-wave may
simply increase in height, and/or the ST segment becomes elevated. The finale
phase is the acute phase. In the acute phase, (usually the first
hour or more) the ST segment elevation is accompanied by the development of a
pathological Q wave. This Q-wave confirms the diagnosis of
MI.
This evolution is not precise, however. Often times the T-wave may invert in
the presence of ST segment elevation during the end of the hyperacute phase. In
any event... the most critical observation should be the recognition of ST
elevation in 2 or contiguous leads. This is most important to paramedic in the
pre-hospital phase because the development of the Q-wave may take hours and
could easily be missed in the field.
Eventually, the ST segment will return to its baseline and the T-wave resumes
its normal position, leaving only the Q-wave as evidence that an infarction has
occurred. Recent research and studies have produced 95% accuracy in field
diagnosis by paramedics. Perhaps some reasons would include other indications
for ST changes. They would include simple angina, drug effects, and electrolyte
imbalance.
Axis Deviation:
Use Lead I, II, and aVF to diagnose Axis
Deviation
Vectors and Axis
- Vector: A quantity of electrical force that has a known magnitude and
direction.
- Axis: A hypothetical line which joins the poles of a lead which measure
electrical force.
- Mean Cardiac Vector: The average of all the instantaneous vectors. (
AKA mean electrical axis ).
-
For pre-hospital purposes, the axis is either "normal"
or "not normal."
- Normal Deviation:
- The QRS deflection is upright or positive in I and either aVF or Lead
II.
- A normal axis means the QRS axis falls between 30 and 90 degrees in the
chest. The heart is lying in an angle between these parameters.
- Right Axis Deviation:
- The QRS is downward or negatively deflected in I and positive in aVF or
Lead II.
- The heart is lying in an angle lower the 30 degrees in the
chest.
Can be normal in young adults or "thin people."
May be
abnormal in people who have a block in the posterior division of the left
bundle.
Can imply delayed activation of the right ventricle ( as seen
in RBBB ) or Right Ventricular enlargement.
Pathology: Right
Ventricular enlargement and hypertrophy. C.O.P.D. Pulmonary Embolism,
Congenital heart Disease, Inferior wall MI.
- Left Axis Deviation:
- The QRS is upright or positively deflection in I and negative in aVF or
Lead II.
- The heart is lying in an angle greater than 90 degrees in the
chest.
Can be normal in the presence of acites, abdominal tumours,
pregnancy or obesity.
Abnormalities are due to Left Ventricular
enlargement or a Left anterior hemiblock.
Pathology: Left ventricular
enlargement, and hypertrophy, Hypertension, Aortic Stenosis. Ischemic Heart
Disease. Inferior wall MI.
As stated above. the electrical current should flow to the positive lead. If
it does not flow in a positive direction, the heart is pointing toward the upper
right or the left. So, if the QRS is negative in aVF, the heart is pointing more
to the left than normal; hence, Left Axis Deviation. If the QRS is negative in
Lead I, the heart is pointing more to the right than normal; hence, Right Axis
Deviation.
This is very complicated and difficult to explain in this forum. If you need
info on AXIS deviation or 12 lead diagnosis, please send E-Mail and information
will be provided by E-Mail or conventional postage.
By, Mitch Mendler E.M.T.
paramedic, San Diego Paramedic.
References:
- Eric Yeargain, Paramedic
- San Diego Paramedic Association field handbook.
- Palomar College, San Marcos, CA. Paramedic Program
 to S.D. Medic 12 lead for more
information...
to S.D. Medic 12 lead for more
information...
More information and educational Software from these
companies:
Genentec
Inc. 
phone #
415-225-1000
Armus Cardiology
Educational Software

phone #
1-800-942-7687
Little Brown
Publishing Company
phone # 1-800-527-0145
Click here to send E-Mail to The
San Diego Medic Association.
To contact Eric Yeargain send him E-Mail here.
Click here to go back to the main page: The San
Diego Medic Association.
 This Ring is owned by Mitch
Mendler.
This Ring is owned by Mitch
Mendler.
[ Ne
xt
Page | Ski
p
It | N
e
xt
5 | Pre
v
|
Random]
Want to join the ring? Get the information
Web page design and maintenance by Mitch Mendler E.M.T.
Paramedic;The WebMaster!
All aspects of this page are copyright © 1996 S.D.M.A.
and unless otherwise stated are property of the San Diego Medic
Association.









 to S.D. Medic 12 lead for more
information...
to S.D. Medic 12 lead for more
information...




